As Nutrition and Hydration Lead at Lulworth House Residential Care Home, I have lots of different responsibilities linked to our residents’ eating capacities and nutrition (including weight loss or gain) and part of that is referring individuals to the Speech and Language Therapy (SLT) and Dietetics team when needed.
At Lulworth House we check all our residents’ weights each month, bi-weekly or weekly as needed and this can help me track any issues which may need external support.
As I have regular contact with each team, I was invited to a recent focus group after I completed a survey for them.
Focus Group and survey discussion
The ‘SLT and Dietetics Mealtimes Focus Group’ was held on Thursday 21 September at Singleton Village Hall. The speakers were Liz Gould from Adult Speech and Language, Kent (ASLT) and Bryony Donaldson, Community Nutrition and Dietetics, Kent who presented the findings of the survey.
Two surveys had been sent out to East and West Kent Care Homes – one concerning swallowing and Speech and Language, and one focusing on nutrition, hydration and Dietetics.
Liz and Bryony started by going through the most common survey answers which showed some of the top issues for Care Home teams, which included long waiting times after referral and not much access to information on what to do during the waiting time. They found that written eating and drinking recommendation sheets from Speech and Language work well and the Dietician or Dietetic Assistants are brilliant at follow ups – whilst getting urgent advice from either team when you have a query or concern doesn’t work well.
They found that 52% of residents from Kent Care Homes referred to SLT, and 55% to the Dietetics, are referred because staff feel it is required for compliance with policies, procedures and CQC. However, staff felt they could manage their residents’ needs with simple changes to their diet or eating habits.
Liz and Bryony have contacted other trusts around the UK to ask if they are experiencing the same issues, only to find that in Kent we have as many as 350 Care Homes Where as other trust areas have closer to 100. Thus referral numbers are high and increasing every year, but despite this SLT and Dietetics services are small, with only one or two clinicians covering local Care Homes as a part of their caseloads. Care Home referrals can make up as much as 30-40% of all the referrals in some areas.
The services’ data seems to show that over 50% of SLT referrals did not need any significant SLT input, whilst the Dietetics team had to reject approximately 400 referrals in a 9-month period in 2022/23.
All in all, there are big challenges for both Care Homes and SLT and Dietetic services in how things are currently working, and they want to work with us in local Care Homes to find a new way forward.
Manual for Mealtimes
Liz and Bryony have been in contact with NHS Lothian in Scotland who use a document called ‘Manual for Mealtimes‘ which was designed in collaboration between SLT and Care Homes. Liz and Bryony have been given permission to adapt it to our Kentish needs as well as introduce a Dietetics part of the form. They are now working hard on this and shared it with us to see what we think about potentially using it in Kent.
Key points:
- The idea of the Manual for Mealtimes is that it will become a general guide for all Care Homes, helping to identify which residents should be referred straight away and who can be supported by Care Home staff following advice in the manual.
- Once a problem with swallowing or nutrition is recognised, Care Home teams will use a ‘problem chart‘ to assess which are the main problem areas to be investigated – these include environment, sensory, position, pain, mouth care, social or cognition.
- The manual then provides a range of things to try to help the resident with these issues – things that Care Home staff often would do to improve the quality of life of a resident; changing cutlery, inviting people to sit together, coloured crockery, food fortification, medication changes or added mouth care.
- Using the new manual will evidence that action has been taken and that the Care Home has run a trial of changes, which either do or do not solve the issue; it will show the proof that the care staff are following the guidelines and enacting changes as recommended in the manual. It is hoped this will become the step before an urgent referral is needed.
- The aim is that it will help staff to know what to put in place immediately to help residents and that it should reduce unnecessary referrals to SLT and Dietetics, allowing them to see the people that have more complex problems and in a much faster timescale. The problem chart and trial of changes record will also provide clear documentation of what staff are doing to support residents in a structured way.
A positive development
Liz and Bryony have already had contact with local CQC inspection team members who felt that the manual would be a brilliant addition to the way Care Homes, SLT and Dietetics work together.
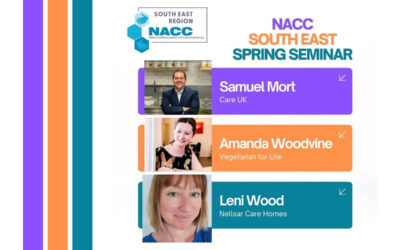
At this time the manual document is in its very early stages and I, along with others in the Focus Group, were given an initial draft version to read through and offer insight. I will also liaise with Nellsar’s Head of Nutrition and Wellness Leni to get her input.
After taking on board our feedback about the manual, they are going to be asking Homes to help pilot the new documentation and then give their feedback on how it works in practice. I of course volunteered to take part straight away and had my hand up before Liz had even finished her sentence!
I’m very much looking forward to seeing these important developments take shape and how we can implement them at Lulworth House and other Nellsar Homes to further improve the wellbeing of our residents.